要約
In this design solution, we consider some of the factors that affect a digital temperature sensor’s ability to continuously and accurately measure human body temperature. After examining some of the limitations of current solutions, we then present a tiny digital temperature sensor IC that will bring several advantages to both medical equipment and wearable device designs of the future.
Introduction
When the global positioning system (GPS) was developed by the U.S. military in the 1970s, few would have envisaged the day when the average civilian would use it in their automobiles or on their smartphones to assist them in navigating their journeys. In a similar vein, clinical-grade sensors that were originally designed to monitor patient health in a hospital setting are increasingly finding their way into a myriad of consumer health and fitness devices (Figure 1).

Figure 1. Wearable technologies of today.
However, the tightly controlled environment of an infirmary is very different to the entropy of daily life. Consequently, the everyday conditions encountered by sensors present in wearable devices provide a very different challenge to those posed to similar sensors operating in hospital equipment. In this design solution, we consider some of the factors that affect the ability to continuously and accurately measure human body temperature using digital sensors. After examining some limitations of current solutions, we then present a tiny digital temperature sensor IC that will bring several advantages to both medical equipment and wearable device designs of the future.
Human Body Temperature
For a healthy person, body temperature is usually in the range of 97°F to 99°F (36.5°C to 37.5°C), although there are many factors that can cause this to vary including age, gender, activity levels, and time of the day (to name a few). Variation in excess of these values for an extended period may be an indication of a relatively common health problem (e.g. fever), while a sudden drop in body temperature in a post-surgery patient may be an indication of a potentially life-threatening condition (e.g. sepsis). Hence, the ability to quickly and accurately measure body temperature is very important to physicians. Originally measured using mercury bulb thermometers (since abandoned for safety reasons), body temperature is now usually measured using a digital thermometer probe.
In addition to the variables previously listed, another factor to consider when measuring temperature is the body location where the measurement is made. In a hospital environment, this is normally done by placing a probe in the ear, mouth, or rectal canal. Interestingly, ear and rectal temperatures are usually higher than oral, which in turn is higher than that of the armpit (also sometimes used). While intermittent temperature measurements taken at these body locations are usually tolerable for immobile patients in a clinical setting, they are nonetheless invasive with the potential to cause small levels of discomfort. For this reason, these body locations are not practical for continuous temperature monitoring using a wearable device.
Skin Measurement
An obvious, easily accessible body location for continuous temperature monitoring is on the skin, which is the largest organ in the human body. Conveniently, most consumer wearables are worn on the wrist (and therefore in contact with skin). However, while temperature measurements taken at this location may be useful to monitor transient variations (for example, those caused by exercise or activity) and daily trends, this is not an ideal location for accurate clinical monitoring. This is due to the distance of the device from the heart and exposure to temporal environmental conditions. Hands have a lower and more variable temperature than the rest of the body.
A more desirable scenario would be to place multiple monitors in contact with the skin at different locations on the body, generating a dataset that can be used to calculate a value more reflective of overall body temperature. Interestingly, recent research has indicated that localized variations in skin temperature may be a marker for disease (e.g. malignant tumors). It is more likely that these local temperature variations are detected when multiple monitors are used.
Temperature Monitor Design
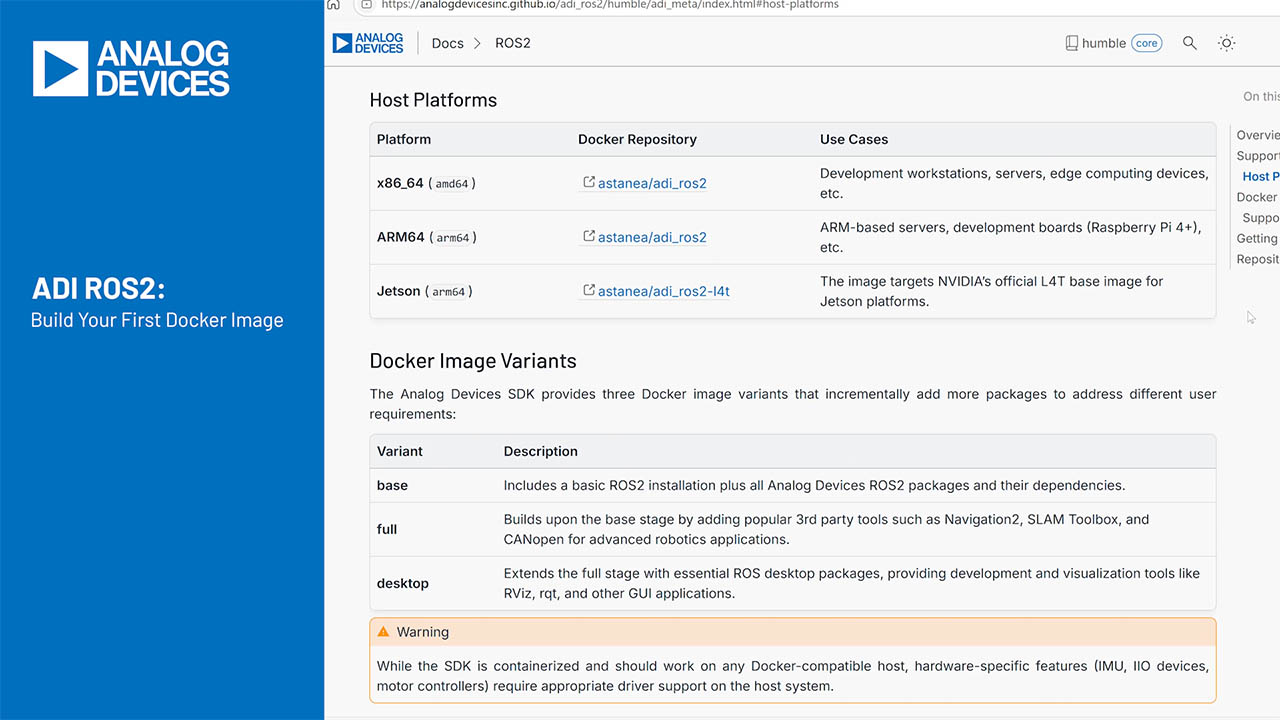
A wearable temperature monitor requires a battery, a microcontroller (suitable for wearable applications), and a temperature sensor IC (Figure 2). To extend battery life for as long as possible, it is essential that both ICs consume as little power as possible. To maximize portability while minimizing discomfort to the wearer, the size of both should be as small as possible. This type of monitor is typically attached to a single location on the body using an adhesive patch.

Figure 2. Building blocks for temperature monitor.
Many temperature sensor ICs have a metal thermal pad located on the underside of the package (Figure 3). Heat is conducted from the body measurement point to the thermal pad which the IC then converts into a digital representation.

Figure 3. Typical temperature sensor IC (bottom view).
The location of this pad can cause two design problems. First, its location underneath the package makes it difficult for the PCB designer to route metal tracks from the point of contact with the body, through the board, and to the pad. Second, due to its close proximity to the other pins on the same IC, there is potential for parasitic self-heating to occur, caused by the heating effect of current flowing into and out of the other pins. This potentially interferes with the desired body temperature measurement.
Apart from these design issues, there is also a practical concern worth considering. Measuring temperature at multiple body locations would require multiple independent instances of the same monitor, each with its own battery (requiring periodic recharging/replacing), microcontroller (from which stored data must be retrieved), and temperature sensor IC. Apart from the obvious inconvenience to the wearer, who must have multiple adhesive patches attached, it is a costly, inefficient, and unwieldy approach.
Daisy-Chain
Figure 4 illustrates a more practical approach to measuring body temperature at multiple locations. The fabric of this close-fitting, sports-type garment incorporates multiple temperature sensor ICs, which are connected in a daisy-chain arrangement to a single battery and host microcontroller. Each temperature sensor can be polled by the microcontroller on a regular basis to create a profile of both local and whole-body temperature.

Figure 4. Garment incorporating multiple temperature sensors.
This arrangement is possible by using the temperature sensor IC shown in Figure 5.

Figure 5. MAX30208 digital temperature sensor.
Apart from its tiny size (2mm x 2mm x 0.75mm), this clinical-grade digital temperature sensor IC has several advantages over other temperature sensors.
Instead of using a thermal pad on the underside of the package, temperature is measured at the top of the package, as far away as possible from its pins, minimizing the potential for parasitic self-heating. As shown in Figure 6, an innovative feature of this part is that it does not require mounting on a dedicated PCB. This means it can easily be connected to a remote host microcontroller using a flat flexible/printer cable (FFC/FPC), allowing multiple sensors to be comfortably embedded and connected together within the fabric of a wearable garment.

Figure 6. Sensor connected to a microcontroller using FFC/FPC.
This sensor is highly accurate to ±0.1°C across the expected human body temperature range (35.8°C to 41°C) and operates across a wide voltage range (1.7V to 3.6V) consuming only 60µA current during measurement and 0.5µA in shutdown. It includes a 32-word FIFO for temperature data (allowing the CPU to sleep for longer) and includes high and low threshold digital temperature alarms. An I2C interface allows multiple parts to connect to a microcontroller in a daisy-chain configuration (Figure 7).

Figure 7. Multi-point temperature sensing using I2C.
Additional sensors can be connected to the daisy chain by using an I2C multiplexer, if required (Figure 8).

Figure 8. I2C multiplexer.
Summary
Continuous, accurate body temperature monitoring of a mobile person requires a very different approach to the intermittent, invasive methods used for a static patient in a clinical environment. It requires wearable temperature monitors located at multiple locations on the surface of the skin, with minimum discomfort for the wearer. When selecting a temperature sensor IC for such an application, the potential for parasitic self-heating caused by the location of the thermal pad on the underside of the package should be kept in mind. As we have shown, this can be avoided by choosing a temperature sensor IC which measures temperature at the top of its package. We also showed that since this IC does not require PCB mounting, it is particularly suitable for use in a remote, multi-sensor configuration within a wearable garment. Other applications for this part include medical thermometers and IoT devices.