Transthoracic Impedance Measurements in Patient Monitoring
Patient monitors measure and display the various vital signs of the connected patient. The main signature of interest is the patient’s electrocardiogram (ECG) signal, but other parameters of interest and importance include temperature, blood pressure, and respiration rate. This article describes the nature of the respiration measurement based on thoracic impedance. The respiratory system supplies our blood with adequate oxygen through breathing. All cells in the body require oxygen to survive, grow, and turn food into energy. When we breathe, we inhale oxygen and exhale carbon dioxide and water vapor as by-products of cellular respiration. Breathing is mostly an involuntary—and usually effortless—process under control of the autonomic nervous system, which instigates contraction and relaxation of the diaphragm and the muscles around the lungs. This contraction and relaxation produces a rhythmic respiratory rate and pattern. Relaxed respiration is constant, interspersed with the occasional yawn or sigh. At rest, only the inspiration muscles are in use, with exhalation usually being a passive process as the lungs rebound after the inhalation stretch.1
Normal respiration depends on a variety of factors such as age, fitness level, and stress level; and is generally at a constant rate and volume. The breath intake for a newborn could be in the range of 30 to 60 breaths per minute, whereas a normal respiration rate for an adult might be around 12 to 20 breaths in that same one minute time frame, increasing with stress, illness, and activity level. More relaxed individuals using breathing techniques or in a meditative state might achieve rates as low as a mere three to five breaths per minute.
In hospital environments, physiological observations of pulse, blood pressure, temperature, respiration, and consciousness levels give physicians and nurses timely information related to patient health. Of these parameters, respiration rate, a critical vital sign that provides important information about patient distress or respiratory issues, is sometimes underutilized.3, 4 An abnormal respiratory rate (in excess of that shown in Table 1), changes in respiratory rhythm, or more effortful breathing may indicate some physiological instability and could help to identify patients at risk of cardiac issues such as CHF (chronic heart failure).5
| Group | Age | Breaths/Min |
| Newborn to six weeks | Newborn to six weeks | 30 to 60 |
| Infant | Six weeks to six months | 25 to 40 |
| Toddler | One to three years | 20 to 30 |
| Young Children | Three to six years | 20 to 25 |
| Older Children | 10 to 14 years | 15 to 20 |
| Adults | Adults | 12 to 20 |
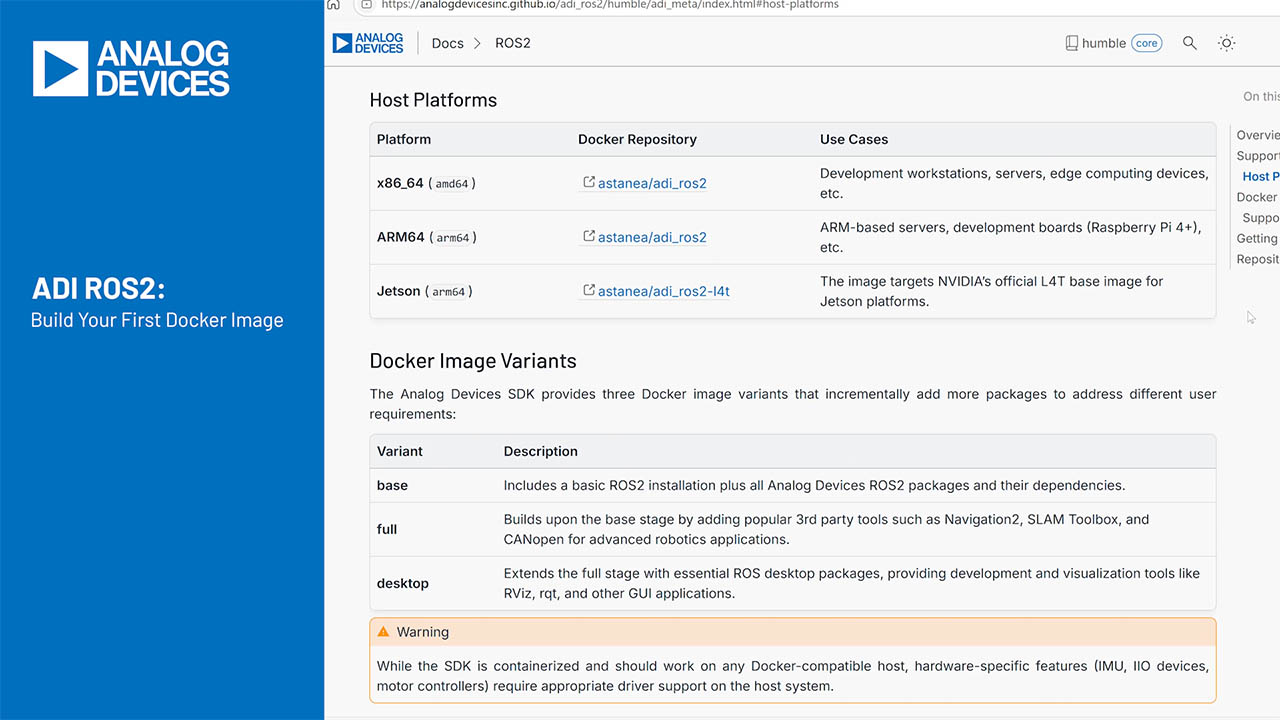
The key to determining the patient’s respiration rate is to measure the changing impedance of the thoracic cavity, which varies with each inhalation and exhalation. The impedance increases as the patient inhales and decreases as he exhales. A circuit designed to detect this impedance variation—based on impedance pneumography—delivers a high frequency differential current driven onto the patient through a pair of electrodes. The impedance variation caused by breathing results in a corresponding voltage change that can be measured on the same electrodes (2-wire respiration measurement), or on a different pair of electrodes (4-wire respiration measurement).
Achieving the optimum respiration measurement can greatly depend on patient position. For example, if the patient is sleeping or in a lying position, breathing tends to be in the abdomen area; so, Lead II or Lead III might provide the best 2-wire measurement. Alternatively, if the patient is in an upright position, a better signal might be available on the Lead I electrode pair. In addition, stress tends to make us breathe only in our upper chest, so Lead II or Lead III might still be the appropriate choice for the calmer individuals among us. A respiration circuit designed to multiplex different pairs of electrodes will ensure full coverage so the best respiration measurement can be captured.

Figure 1. Physical Electrode Placement for Limb Leads and Lead Configuration.
Drive Circuit
A typical arrangement consists of a drive-and-measure circuit. The drive portion may be a DDS or a DAC that delivers the two out-of-phase ac-coupled currents at the programmed frequency onto the pair of electrodes. The current is driven onto the patient using series resistors and capacitors. The ac coupling serves to isolate the patient from dc, alleviating any concerns around supplying common-mode voltage to the patient. The value of the ac-coupling capacitors determines the current amplitude. Larger capacitor values increase the drive current, which results in larger voltage differentials that can increase the signal-to-noise ratio. Figure 2 illustrates a typical signal chain showing the respiration drive and measurement circuits.

Figure 2. Typical Signal Chain for Impedance Pneumography Measurement, Showing Drive and Measure Paths.
Medical standards dictate the maximum allowable current that may be safely injected into a patient, starting at 50 μA rms from dc to 1 kHz. The allowable current doubles for every doubling in frequency, increasing to 1 mA at 100 kHz, and then leveling off. If the respiration function is sharing the same electrodes as an ECG circuit, then the patient auxiliary current limit is 10 µA at dc.
The drive frequency is typically above 20 kHz, as the skin-to-electrode impedance decreases by a factor of about 100 as the frequency increases from low values up to 100 kHz. Frequencies above 100 kHz are not common for respiration drive, as stray capacitances can be difficult to control and interferers such as surgical equipment become problematic.

Figure 3. Patient Skin Impedance vs. Frequency6.
The impedance between the carrier electrodes is the sum of the cable resistance, including any defibrillation-protection resistors present in each electrode (RCABLE typically 1 kΩ to 10 kΩ, greater for some cables), the electrode-to-skin interface impedance (50 Ω to 700 Ω), and the body’s bulk-tissue impedance between the electrodes (RTHORACIC approximately 100 Ω to 500 Ω). In the presence of these large static impedances, the measurement circuit must resolve small sub-ohm variations in the body impedance that occur during a breath (ΔR typically 0.2 Ω to 5 Ω pk-pk). Figure 4 illustrates the contributing impedances distributed along the path to the patient.

Figure 4. Impedance Path to the Patient Including Drive Components.
Measurement Circuit
The measurement portion of this circuit consists of high-pass filtering, amplification, anti-aliasing, analog-to-digital conversion, and synchronous demodulation in the digital domain, as shown in Figure 2. The acquired signal is an amplitude-modulated carrier at the driving frequency, with a shallow modulation envelope at the respiration frequency. Figure 5 shows what this might look like in the time domain. The carrier modulation is small, placing tight constraints on the contributing noise sources and necessitating creation of the largest possible signal. The magnitude of the carrier and the respiration envelope are dependent on the voltage produced by the drive circuit, the value of the thoracic static and dynamic respiratory impedances, and the total resistance between the outputs of the driver circuit. The measurement resolution is limited by the available signal-to-noise ratio. As already discussed, the electrical impedance of the thoracic cavity varies during breathing, with variations of about 0.2 Ω around a baseline of as much as 10 kΩ (total cable impedance in drive and return paths). This produces approximately 2 μV of variation from a 300 mV signal, so either a very high resolution ADC or oversampling is required.

Figure 5. Modulation Envelope Corresponding to Breathing Rate.
Electrodes in contact with the skin, which form a simple battery, can exhibit half-cell potentials of as much as 300 mV each. A high-pass filter removes the dc signal component and allows more ac gain. After anti-aliasing, an ADC digitizes the signal. The digitized signal is multiplied by the I and Q phases of the signal generator, and the results are low-pass filtered to obtain the magnitude of the signal components that are in phase and in quadrature with the signal generator. Since respiration occurs at low frequencies, these low-pass filters can have a cut-off frequency in the tens of Hertz range. The I-Q signal can be converted to magnitude-phase format or used directly by the host processor for further filtering, respiration rate extraction, and analysis.
Analog Devices’ ADAS1000 addresses the many challenges involved with designing a respiration measurement circuit. This chip, primarily a multichannel ECG front end, also offers a complete respiration circuit with both drive and measure functionality. The ADAS1000 provides a flexible respiration arrangement, allowing drive and measurement to be switched across different paths (Lead I, Lead II, and Lead III) to ensure that the best possible respiration signal can be detected. It also supports the option of separating the respiration “drive” and “receive” paths, as shown in Figure 6, to provide greater drive than might be possible through the ECG cables. This can be useful for measuring respiration during motion, when the measurement may benefit from driving one set of electrodes and measuring another. Such an approach could use an arrangement where the carrier is injected onto Lead I, for example, while the measurement is made on a different set of electrodes (4-wire arrangement).

Figure 6. ADAS1000 Showing Flexible Respiration Switching.
A 4-wire/electrode measurement can significantly enhance the overall resolution for cases when higher resolution (<0.2 Ω) is required. Injecting the impedance carrier on Lead I with external drive capacitors and measuring the respiration signal on a different set of electrodes, such as LL relative to RL, gives the ability to resolve much lower levels of impedance. Other configurations may take advantage of other electrode combinations.
Conclusion
Patient respiration measurement is a key parameter used alongside other important vital signs by healthcare professionals. This article defined the signal of interest and one approach to measuring this vital sign. The recently released ADAS1000 offers an integrated solution to measuring not only ECG signals, but respiration as well, adding value and simplifying the design of vital sign monitoring equipment.